
Can Chronic Pain Be Cured In 2024?
Many individuals grapple with relentless chronic pain, seeking a definitive cure. Chronic Pain Focus examines various conditions such as complex regional pain syndrome and the relationship between persistent discomfort and emotional well-being. People often find themselves caught in an exhausting cycle of pain management techniques that range from physical therapy to more invasive procedures like surgery, yet relief remains elusive for some. The intriguing idea posed by recent literature suggests psychological factors may influence one’s experience of physical pain, proposing a mind-body connection where emotions like anxiety or depression could manifest as physical symptoms.
Understanding Chronic Pain
Chronic pain grips the body for long stretches. It lives far past normal injury healing, lasting months or years. Living with it means a constant fight; the ache never winks out on its own.In some cases, like that reported by Justin J Wee in The New York Times, traditional fixes fall short – physical therapy and even surgery offered him no respite from his enduring piriformis muscle torment. Chronic discomfort is often part of daily life without clear reasons in scans or X-rays. Sarno of NYU linked hidden anxieties and repressed anger to this persistent state. Embracing such a perspective heralds an inward journey. Documenting angst-ridden thoughts may unravel mental strain knots, offering relief beyond medicine’s reach.
Exploring Cure Possibilities
In the quest to cure chronic pain, doctors often look at both new and established treatments. Research has shown that certain drugs can help by changing how nerves carry pain signals. For some patients, this may offer relief when other options fail.Physical therapy is another key approach; it strengthens muscles and improves flexibility which might lessen discomfort over time.
Meanwhile, technological advances have introduced high-tech solutions like nerve stimulation devices. These small machines send electrical pulses to disrupt painful sensations before they reach the brain.Every case differs though—what works for one person might not suit another. So treatment plans are as unique as fingerprints, tailored just for each patient’s needs.
Managing Long-Term Discomfort
Managing long-term discomfort hinges on regular, small actions rather than quick fixes. One might start with daily gentle exercises like walking or swimming to maintain mobility and ease pain. Health professionals also suggest incorporating anti-inflammatory foods into one’s diet; think fish, nuts, and leafy greens which can help reduce swelling in tissues.Over time these lifestyle choices may lessen the ache that comes with chronic conditions such as arthritis or back issues. It’s not a cure. For many, it eases life without constant medication.
Complex Regional Pain Syndrome Insights
Complex Regional Pain Syndrome (CRPS) often starts with a trauma or surgery. Patients, mainly women over 18, face swollen limbs and intense pain that can turn ‘cold’ within months. Delays in recognizing CRPS lead to worse health and life quality. Treatment blends physical therapy, drugs like antidepressants and ketamine, plus psychological support such as cognitive behavioural therapy (CBT).
The Budapest Criteria help diagnose it more clearly – crucial for improved outcomes since late treatment means therapies might not work well. Despite some strong drug evidence, overall scientific backing is weak; hence results vary greatly among patients struggling with this enduring condition.
Anxiety and Its Role in Pain
Anxiety, tightly linked with pain, can heighten the feeling of it. This link isn’t just in one’s head; rather, it stems from shared biological pathways. In areas where we feel and react to pain—the amygdala or hypothalamus—these also relate to anxiety and depression.A person who feels anxious may thus experience more intense pain symptoms due a double effect on their nervous system. Treating this mesh of discomfort gets tricky for doctors as signs often overlap each other making diagnosis hard. Cognitive Behavioural Therapy (CBT) shows promise here by tackling both emotional distress while easing chronic physical pains too..
Depression Linked with Persistent Ache
Persistent pain often walks hand in hand with depression. People who live with unending ache carry a heavy burden, not just physically but also emotionally. The stress of long-term discomfort can alter the brain’s and nervous system’s chemistry, impacting mood and thoughts.It’s these changes that may trigger depression for some sufferers. Daily pain can make work or home life a struggle. Social activities and hobbies often suffer due to chronic pain, which is four times more common alongside anxiety or depression.
Everyday tasks become mountains as sleep falters, energy dips, focus blurs, appetite wanes and moods swing unpredictably under chronic pain’s shadow—fueling further despair and distress within an individual. This cycle where physical agony amplifies emotional turmoil creates a challenging reality where both body and mind suffer severely.
Holistic Approaches to Alleviation
Holistic approaches target pain at its roots. They blend mind and body practices to ease discomfort. For example, acupuncture opens up blocked energy flow; studies show it cuts pain by half in some people.Yoga stretches muscles gently, easing tension that can lead to aches. Meditation calms the brain which may lower how much we feel hurt. Diet changes reduce inflammation inside our bodies that often causes chronic suffering.All these elements work together not just for momentary relief but for long-term wellness too. Holistic care offers hope as part of an overall plan alongside traditional medicine’s help when trying to cure persistent pain issues.
Medical Interventions for Relief
Medical interventions to ease chronic pain vary in scope and duration. Radiofrequency ablation, or RFA, is one such treatment that can lessen discomfort from 8 months up to a year; studies are examining if its cooled form offers heightened benefits. When pain persists after this period, repeat treatments remain an option.
Injection therapies provide temporary relief ranging from weeks to a full year—multiple sessions might be needed for sustained effect. For enduring respite, specialists like Dr. Finkelstein propose the use of implanted pain pumps which release medication automatically near the spine.
In cases where medications are essential, opioids may be prescribed cautiously due to their potency but have shown effectiveness particularly with lower back and joint pains stemming from arthritis conditions. Meanwhile complementary practices like massage or yoga offer alternative options though their effects could last shorter periods—it’s vital patients consult doctors when considering these approaches as adjunctive therapy.
It’s important too that treatment plans focus not solely on curbing discomfort but enhancing life quality overall—a primary goal underscored by experts including Dr Yoon at Los Angeles’ Kerlan-Jobe Orthopaedic Clinic specializing in joint issues and sports injuries.
Lifestyle Adjustments for Improvement
People with long-term pain can change their way of life to improve how they feel. One should move more; even gentle walks help muscles and minds. Eating well also matters, as good food aids body healing.Less sugar plus more water keep weight in check, easing strain on joints. Sleep heals too—aim for eight hours a night with regular bedtimes and wake-up calls ensuring restful nights that assist recovery during the day.
Psychological Therapies Explained
Psychological therapies for chronic pain work by changing thought patterns. These treatments, including cognitive behavioural therapy or short CBT, challenge negative thoughts that can make pain worse. They help build new ways of thinking and reacting to pain. Experts guide patients through this process safely; it’s a key part of care plans today.
Over time, these methods have proven effective in reducing both the intensity and impact of ongoing pain on life. With regular sessions led by trained therapists, many find they regain control over their discomfort without needing more drugs or surgery — a real step forwards in managing well-being.
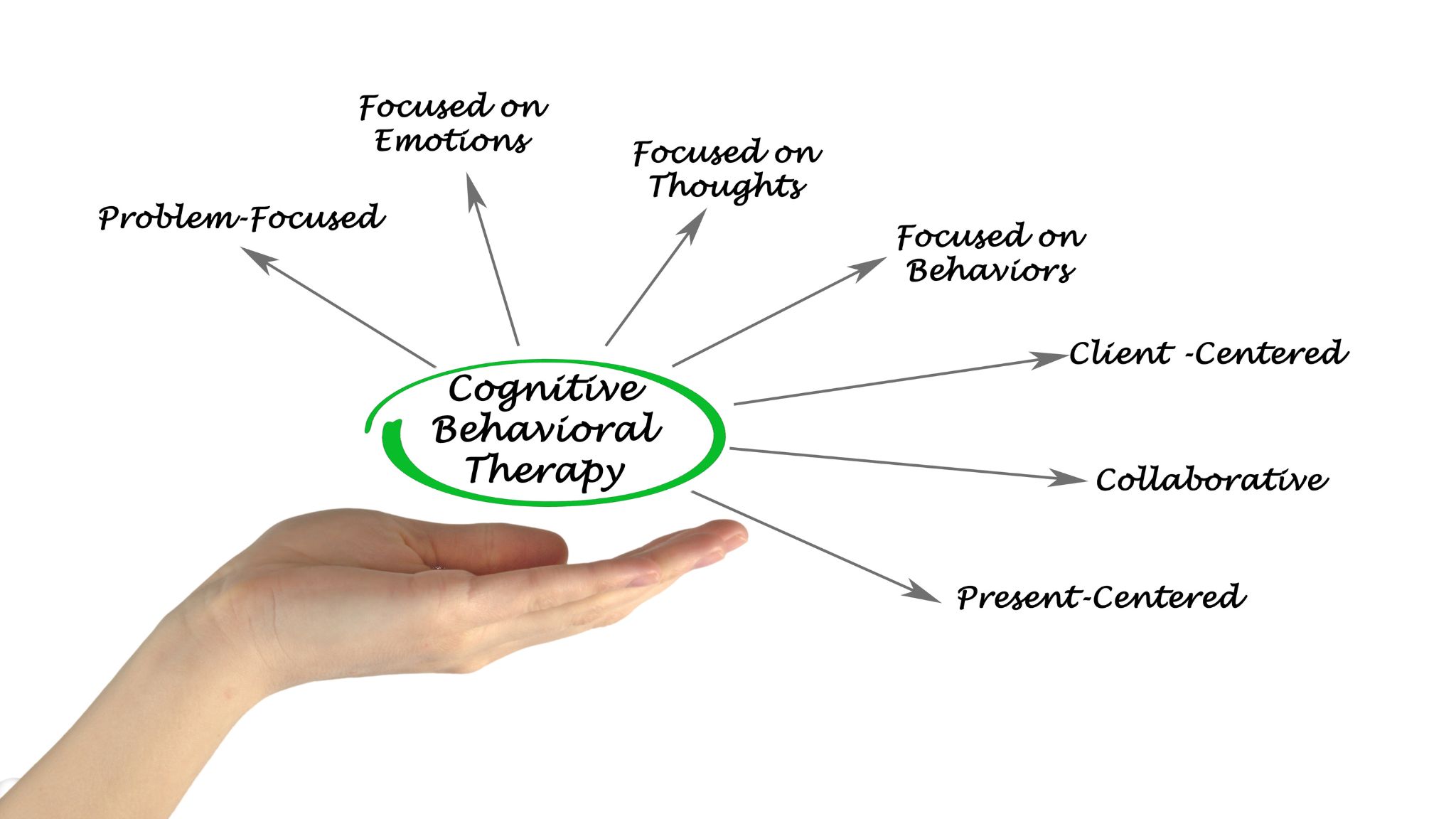
Support Networks and Coping Strategies
Support networks play a pivotal role in managing chronic pain. Friends, family, and others facing similar challenges form a web of support that can offer comfort and practical help. Emotionally, this network gives strength when pain feels overwhelming. Effective coping strategies include cognitive-behavioural therapy (CBT), aiding individuals to reframe negative thoughts which might amplify their discomfort or lead to depression and anxiety. CBT encourages more positive outlooks alongside relaxation techniques to calm the mind. Activation methods uplift mood through gentle activity while operant training builds up tolerance incrementally without triggering excessive pain flare-ups.
Together with psychological guidance, patients learn distraction skills reducing focus on distress thanks to interceptive exposure—facing sensations they fear in controlled ways—to lessen overall disability caused by persistent pain syndromes. Chronic pain presents a complex challenge; complete cure remains elusive. Treatment focuses on managing symptoms and improving quality of life, rather than curing the condition outright. Advances in medicine offer hope for better management strategies, yet patients often require personalised care plans that address physical discomfort alongside emotional well-being.
Research continues to evolve, deepening our understanding of how chronic pain affects individuals differently. This necessitates the ongoing adaptation of therapeutic approaches to effectively meet each unique need, striving for a future where enduring relief is attainable for all sufferers.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10265428/
Five things I wish I knew earlier in my journey with chronic pain