Chronic Pain and Mental Health
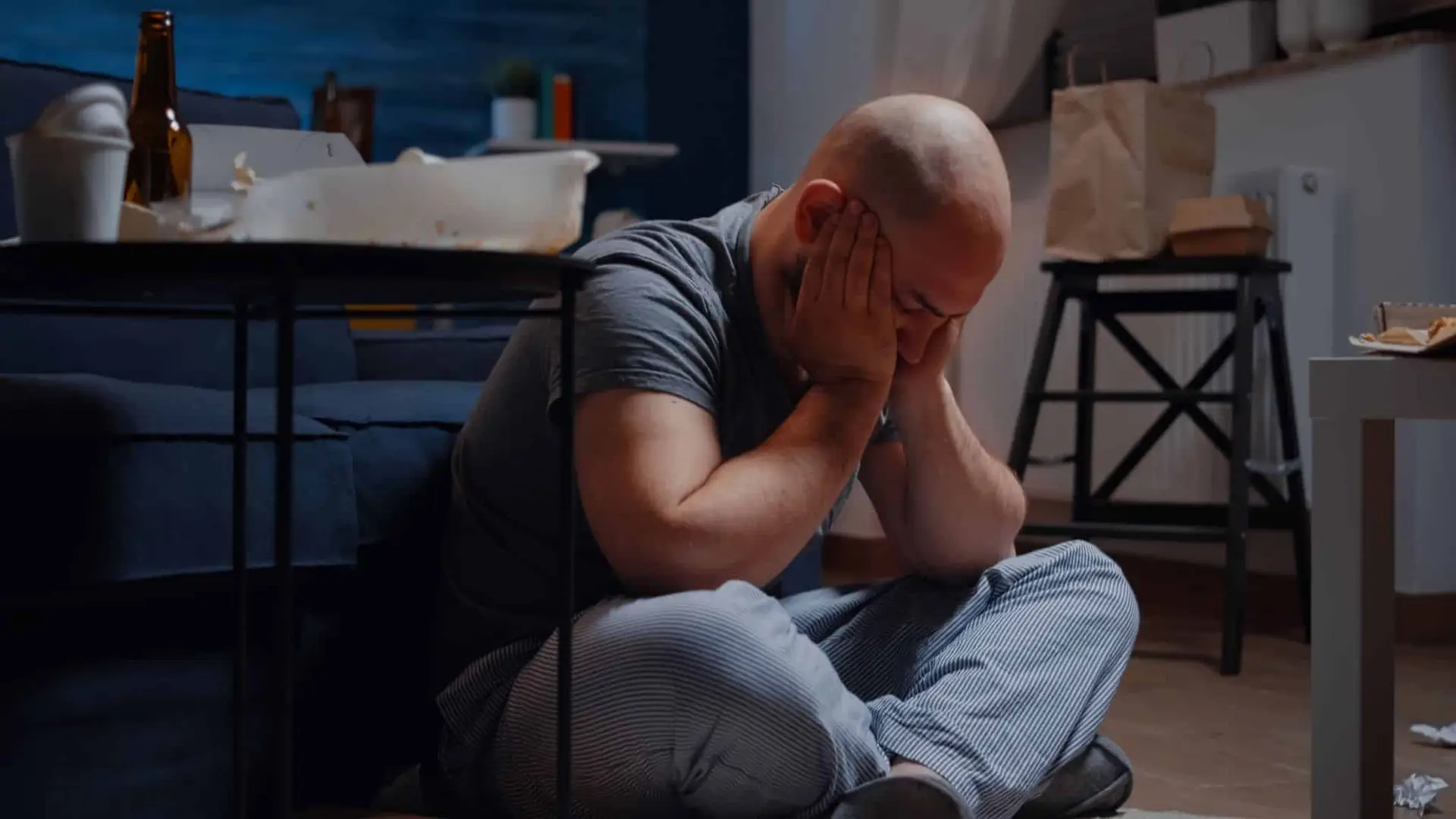
Chronic pain is much more than a physical burden; it weaves most of the time into the very breadth of our emotional and mental well-being. Living with persistent pain can be exhausting and frustrating; it can leave one helpless—helpless enough to drive one to depression or anxiety. With your body constantly firing pain signals into your brain, it isn’t easy to have a good outlook on life.
Long-standing pain and mental health often go hand in hand; how to understand the interplay between them is part of managing both. The constant physical discomfort may interfere with your sleep, lessen participation in activities you have previously enjoyed, and put pressure on relationships. This spiral downward can often invoke feelings of having your mental health slipping, and because of this, the pain feels worse—but these feed into some cycle that seems almost impossible to stop.
In essence, managing chronic pain and mental health is about finding a balance that works for you. It’s a journey that requires patience, self-compassion, and a willingness to explore various strategies to discover what brings you the most relief and joy. Remember, every step you take towards understanding and addressing the interplay between pain and mental health is a step towards a more fulfilling life.
Understanding the Connection Between Chronic Pain and Depression
Chronic pain and depression are intricately connected, with each condition often exacerbating the other. Studies have shown that individuals suffering from long-term physical pain are more susceptible to developing depression due to the ongoing emotional and mental strain. This connection is rooted in shared biological mechanisms, such as disruptions in neurotransmitter function. The persistence of pain can lead to chemical changes in the brain, intensifying feelings of sadness and hopelessness. Recognising this link is crucial for both patients and healthcare providers to create effective treatment plans that address the whole person, not just isolated symptoms.
The Vicious Cycle: How Depression Intensifies Chronic Pain
The relationship between chronic pain and depression is a two-way street. While chronic pain can trigger depressive symptoms, depression itself can worsen the experience of physical discomfort. When someone is depressed, their perception of pain becomes heightened, leading to an endless cycle of physical and emotional suffering. This feedback loop emphasizes the importance of integrated treatment strategies that target both pain relief and mental health care. Approaches like cognitive-behavioral therapy, medication, and lifestyle modifications can help break this cycle and provide patients with lasting relief.
Holistic Approaches to Managing Chronic Pain and Depression
Managing chronic pain and depression requires a comprehensive, holistic approach. Research suggests that combining physical and psychological therapies can significantly improve outcomes for individuals dealing with these interconnected conditions. Treatment plans may include physical rehabilitation, mindfulness practices, and psychotherapy to address both the body and mind. Additionally, building a strong support system can help patients navigate the challenges of chronic pain and depression. By understanding the importance of holistic care, patients and providers can work together to improve overall well-being and life satisfaction.
The Complex Link Between Chronic Pain and Anxiety Disorders
Chronic pain and anxiety disorders are deeply interconnected, creating a complex relationship that affects millions worldwide. Persistent pain not only causes physical discomfort but also leads to heightened anxiety levels as individuals worry about their condition and future well-being. This anxiety can amplify the sensation of pain, making it feel more intense and harder to manage. Research has found that the overlap between these two conditions is due to shared neurological pathways that regulate both pain and emotional responses. Understanding this link is essential for developing effective treatment strategies that address both physical and psychological aspects of the patient’s experience.
How Anxiety Disorders Influence Pain Perception
Anxiety disorders can significantly alter the perception and experience of chronic pain, making pain management even more challenging. When a person experiences high anxiety, their body is in a state of heightened alertness, which can increase pain sensitivity. This heightened state triggers the release of stress hormones, exacerbating inflammation and intensifying physical discomfort. As a result, people with anxiety disorders often report more severe pain and struggle to find relief through conventional pain management methods. Addressing anxiety through therapies such as cognitive-behavioural therapy or mindfulness techniques can help reduce pain perception and improve overall quality of life.
Holistic Treatment Approaches for Pain and Anxiety
Managing chronic pain and anxiety disorders effectively requires a holistic treatment approach that considers the whole person. Combining physical pain management strategies with anxiety-reducing techniques can lead to better outcomes. For example, incorporating mindfulness-based stress reduction, relaxation techniques, or therapeutic exercises can help patients gain control over their anxiety and, in turn, manage their pain more effectively. Additionally, working with mental health professionals to develop coping strategies can significantly improve emotional well-being. An integrated care plan that addresses both chronic pain and anxiety provides a pathway toward long-term healing and improved daily functioning.
Mindfulness Meditation for Stress and Pain Relief
Mindfulness meditation is a powerful technique for managing stress related to chronic pain. This practice involves focusing on the present moment and accepting feelings without judgment. By engaging in mindfulness, individuals can reduce the mental and emotional distress that often accompanies chronic pain. Studies have shown that regular meditation can lower stress hormones, decrease anxiety, and improve overall pain tolerance. Techniques such as guided meditation, body scans, and deep breathing exercises can be integrated into daily routines, providing a sense of calm and enhancing the body’s natural healing processes.
The Benefits of Physical Activity for Stress Reduction
Engaging in gentle physical activity is another effective method for reducing stress caused by chronic pain. Activities like yoga, tai chi, and walking can help release endorphins, the body’s natural painkillers, while also easing muscle tension. Regular exercise has been found to improve mood, decrease stress levels, and increase flexibility, which is particularly beneficial for individuals with chronic pain. Low-impact workouts tailored to an individual’s physical capabilities can be especially effective. Consulting a physical therapist or healthcare provider can help develop a safe exercise plan that promotes both physical and mental well-being.
Cognitive-Behavioural Techniques to Manage Stress
Cognitive-behavioural techniques (CBT) are evidence-based strategies that can help individuals manage stress related to chronic pain. CBT focuses on changing negative thought patterns and behaviors that exacerbate stress and discomfort. By learning to reframe thoughts and respond to pain in a more constructive way, individuals can reduce their emotional and physical suffering. Techniques such as journaling, setting realistic goals, and practicing self-compassion are essential components of CBT. Seeking guidance from a licensed therapist can help tailor these strategies to fit each person’s unique experience, providing lasting benefits for stress and pain management.
How CBT Alleviates Chronic Pain
Cognitive Behavioural Therapy (CBT) has proven to be an effective approach for managing chronic pain. By addressing the connection between thoughts, emotions, and physical sensations, CBT helps individuals develop healthier responses to pain. Through CBT, patients learn to recognize and challenge negative thought patterns that can amplify their perception of pain. Techniques such as thought reframing and cognitive restructuring empower individuals to reduce the emotional impact of pain, ultimately leading to a more manageable and positive outlook. This method has shown significant success in not only reducing pain intensity but also enhancing quality of life.
CBT’s Role in Improving Mental Health
CBT is also a valuable tool for improving mental health, particularly for those struggling with anxiety and depression related to chronic pain. The emotional distress caused by ongoing physical discomfort can lead to a cycle of negative thinking and heightened stress. CBT breaks this cycle by teaching patients how to control their responses and manage emotional triggers. By practicing mindfulness and focusing on practical solutions, individuals can reduce anxiety, boost mood, and foster resilience. The structured nature of CBT provides a clear pathway for mental health improvement, making it a widely recommended therapy by mental health professionals.
Practical CBT Techniques for Pain and Mental Health
Several practical CBT techniques are used to address pain and mental health challenges. One common method is the use of relaxation exercises, which can help decrease muscle tension and stress. Another effective strategy is the use of activity pacing, where patients learn to balance rest and activity to avoid pain flare-ups. Additionally, CBT often includes goal-setting and journaling to track progress and celebrate small victories. These techniques empower individuals to take an active role in managing their well-being, making CBT a comprehensive and adaptable approach for both pain relief and mental health enhancement.
The Power of Mindfulness in Alleviating Chronic Pain
Mindfulness practices are increasingly recognized for their effectiveness in managing chronic pain. By focusing on the present moment and observing sensations without judgment, mindfulness can help reduce the intensity of pain. Research shows that mindfulness meditation lowers pain perception by altering the way the brain processes pain signals. Techniques like body scanning and mindful breathing create a greater sense of bodily awareness and relaxation, helping to break the cycle of pain and stress. Practicing mindfulness regularly can lead to long-term pain relief and enhance overall physical comfort.
Mindfulness Techniques to Boost Mental Health
In addition to physical benefits, mindfulness practices significantly improve mental health by reducing symptoms of anxiety, stress, and depression. By cultivating awareness and acceptance, mindfulness helps individuals manage emotional reactions and develop healthier coping mechanisms. Meditation, gratitude journaling, and mindful walking are practical ways to reduce negative thinking patterns and promote a sense of inner peace. These techniques help to balance emotions, enhance focus, and foster a more positive mindset. Consistent mindfulness practice can lead to lasting mental well-being and greater emotional stability.
Integrating Mindfulness into Daily Routines for Lasting Benefits
Incorporating mindfulness into daily routines is key to experiencing its full benefits for both pain and mental health. Simple practices like taking mindful breaks, focusing on breathwork, or practicing mindful eating can make a significant difference. Even dedicating a few minutes each day to guided meditations can help reduce pain and improve mood. Mindfulness-based stress reduction (MBSR) programs have been particularly effective for individuals dealing with chronic pain and mental health challenges. By integrating mindfulness seamlessly into everyday life, people can achieve better stress management, improved pain tolerance, and a greater sense of overall well-being.
Understanding the Link Between Chronic Pain and PTSD
Chronic pain and post-traumatic stress disorder (PTSD) often co-occur, creating a complex relationship that can make both conditions more difficult to manage. Studies have found that individuals with a history of trauma are more likely to experience chronic pain, as traumatic events can cause lasting changes to the nervous system. This connection is believed to be due to the body’s heightened stress response, which can lead to persistent pain and physical discomfort. Recognising the link between chronic pain and PTSD is crucial for providing holistic and effective care, as treating one condition without addressing the other may yield limited results.
The Impact of PTSD on Chronic Pain Perception
PTSD significantly influences the perception and severity of chronic pain. People with PTSD often experience heightened pain sensitivity due to the hyperarousal and stress associated with their trauma. The constant state of alertness can exacerbate inflammation and muscle tension, making pain symptoms worse. Additionally, flashbacks and intrusive memories can trigger physical reactions that increase discomfort. Understanding how PTSD amplifies pain helps healthcare professionals develop better management strategies. By addressing both the psychological and physical aspects of pain, patients can experience relief and improve their quality of life.
Integrated Treatment Approaches for Chronic Pain and PTSD
Effective management of chronic pain and PTSD requires an integrated treatment approach that addresses both conditions simultaneously. Techniques such as trauma-focused therapy, cognitive-behavioural therapy (CBT), and mindfulness-based practices have proven successful in alleviating symptoms. Combining psychological support with pain management strategies, like physical therapy and medication, can provide comprehensive relief. Holistic approaches that consider the mind-body connection are particularly beneficial for patients dealing with both chronic pain and PTSD, helping them reclaim their sense of well-being and improve their overall functioning.
The Connection Between Chronic Pain and Sleep Disorders
Chronic pain and sleep disorders are often closely linked, with each condition negatively impacting the other. Persistent pain can make it difficult to fall or stay asleep, leading to poor sleep quality and chronic fatigue. Sleep deprivation, in turn, can worsen the experience of pain, creating a cycle that is challenging to break. Research shows that disrupted sleep exacerbates pain sensitivity, reducing the body’s ability to heal and recover. Understanding this relationship is crucial for developing effective strategies to manage both chronic pain and sleep disturbances simultaneously, as proper sleep is essential for overall health and well-being.
The Mental Health Consequences of Sleep Disorders and Pain
Sleep disorders associated with chronic pain can have a significant impact on mental health. Poor sleep quality is linked to increased rates of anxiety, depression, and emotional distress. When individuals experience long-term sleep deprivation, their brain’s ability to regulate mood and stress responses is compromised. This can lead to feelings of irritability, hopelessness, and difficulty concentrating. Addressing sleep issues is, therefore, a critical component of managing mental health for those suffering from chronic pain. By improving sleep patterns, individuals can reduce the risk of developing severe mental health conditions and enhance their quality of life.
Strategies to Improve Sleep and Manage Pain
Managing sleep disorders related to chronic pain requires a holistic approach. Techniques such as cognitive-behavioral therapy for insomnia (CBT-I), relaxation exercises, and establishing a consistent sleep routine can help improve sleep quality. Additionally, pain management strategies like gentle stretching, medication, or the use of supportive bedding can ease discomfort at night. Creating a calming sleep environment, free from distractions, is also essential. Combining these methods with stress-reduction practices like mindfulness and meditation can promote better sleep and mental well-being. By addressing both pain and sleep disturbances, individuals can experience improved overall health and emotional balance.
The Psychological Impact of Social Isolation on Chronic Pain Patients
Social isolation can significantly affect individuals suffering from chronic pain, worsening both their physical symptoms and mental health. Being cut off from social interactions often leads to feelings of loneliness, anxiety, and depression, which can exacerbate the perception of pain. The lack of social support deprives sufferers of emotional encouragement, making it difficult to stay motivated in managing their condition. Studies have shown that chronic pain sufferers who feel isolated are more likely to experience heightened pain levels and reduced quality of life. Understanding the deep psychological toll of isolation is crucial for addressing the holistic needs of those in chronic pain.
The Vicious Cycle of Pain and Social Withdrawal
Chronic pain often creates a vicious cycle where pain leads to social withdrawal, and isolation, in turn, worsens the pain experience. People with chronic pain may avoid social activities due to mobility issues, fatigue, or fear of judgment, leading to further isolation. This withdrawal reduces opportunities for joy, connection, and emotional support, which are crucial for coping with pain. As social networks shrink, the emotional burden intensifies, creating a feedback loop that is challenging to escape. Breaking this cycle requires awareness of how isolation and pain interact and proactive strategies to foster meaningful connections.
Strategies to Combat Social Isolation for Chronic Pain Sufferers
Combating social isolation is vital for improving the well-being of chronic pain sufferers. One effective strategy is to stay connected through support groups, either in person or online, where individuals can share experiences and gain encouragement from those who understand their struggles. Engaging in hobbies or activities that provide a sense of purpose and community, such as book clubs or gentle exercise classes, can also help alleviate feelings of loneliness. Additionally, prioritising regular check-ins with friends and family, even through virtual means, can maintain strong social bonds. By actively seeking out support and nurturing relationships, chronic pain sufferers can improve their mental and physical health.
The Emotional Toll of Chronic Pain
Chronic pain goes beyond physical discomfort, significantly impacting an individual’s emotional well-being. Constant pain can lead to feelings of frustration, hopelessness, and even depression as people struggle to cope with the limitations imposed on their daily lives. The stress of managing unrelenting discomfort often disrupts sleep patterns and diminishes quality of life, contributing to emotional instability. Furthermore, chronic pain sufferers may experience a sense of isolation, as their condition prevents them from engaging fully in social and recreational activities. This cycle of physical and emotional distress underscores the importance of addressing emotional health alongside pain management.
How Chronic Pain Fuels Anxiety and Depression
Living with chronic pain can trigger anxiety and depression, making it harder to manage both emotional and physical symptoms. The uncertainty about the future and the inability to control pain episodes can heighten anxiety, while feelings of sadness and despair become common as pain disrupts goals and aspirations. Over time, this emotional strain can affect relationships and decrease overall happiness. The interplay between chronic pain and mental health challenges highlights the necessity of holistic treatment plans. Acknowledging the psychological impact of chronic pain helps healthcare providers develop comprehensive care strategies that promote emotional resilience.
Strategies to Enhance Emotional Well-Being
Improving emotional well-being for chronic pain sufferers involves a multifaceted approach. Techniques like mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can reduce stress and promote mental clarity. Cognitive-behavioural therapy (CBT) is particularly effective, helping individuals reframe negative thought patterns and develop healthier coping mechanisms. Building a strong support network of friends, family, or fellow patients can also foster a sense of community and reduce feelings of isolation. Additionally, engaging in gentle, enjoyable activities, such as art, music, or nature walks, can uplift the spirit and provide meaningful distractions from pain. By prioritising emotional self-care, chronic pain sufferers can improve their overall quality of life.
Emotional Support and Shared Understanding
Support groups play a crucial role in improving the mental health of individuals living with chronic pain. These groups offer a safe space where members can share their experiences, challenges, and successes, fostering a sense of camaraderie and understanding. Knowing that others are facing similar struggles can help alleviate feelings of isolation and loneliness that often accompany chronic pain. The emotional support from fellow members provides validation and encouragement, making it easier for individuals to cope with their pain and mental health challenges. This sense of community can be a powerful tool for emotional healing.
Access to Practical Coping Strategies
One of the significant benefits of participating in support groups is gaining access to practical coping strategies and resources. Members often exchange tips on pain management techniques, mindfulness practices, and self-care routines that have worked for them. These shared experiences can provide valuable insights and new approaches to managing pain and stress. Many support groups also invite guest speakers, such as healthcare professionals, who offer expert advice on managing symptoms and improving quality of life. By learning from others, members can feel more empowered and equipped to take control of their well-being.
Reducing Anxiety and Building Resilience
Support groups can significantly reduce anxiety and boost resilience among individuals dealing with chronic pain. Regularly engaging with others who understand their struggles helps members develop a more positive outlook and a sense of belonging. This social connection can buffer against the emotional toll of chronic pain, providing a network of people who offer hope and strength. Additionally, witnessing the progress of others who have successfully managed their symptoms can be incredibly motivating. The shared experiences and mutual support found in these groups can help members build emotional resilience, making it easier to face daily challenges with a more hopeful and proactive mindset.

The Impact of Chronic Pain on Cognitive Function
Chronic pain doesn’t just affect the body; it has profound effects on the brain, too. Research reveals that persistent pain can lead to deficits in cognitive function, impacting areas like memory, attention, and decision-making. These cognitive challenges often arise because chronic pain activates neurological pathways that interfere with normal brain function. For individuals experiencing ongoing discomfort, understanding this connection is vital for addressing both physical and mental health concerns.
How Pain Alters Brain Structure and Function
Neurological studies have shown that chronic pain can induce structural changes in the brain. The prefrontal cortex and hippocampus, areas critical for cognitive processing, often show signs of shrinkage and altered activity patterns in individuals with long-term pain. This disruption contributes to difficulties in concentration, impaired working memory, and slower cognitive speed. Recognising these changes emphasizes the need for comprehensive treatments that not only alleviate pain but also protect brain health.
Strategies for Managing Cognitive Decline in Chronic Pain Patients
Managing cognitive decline associated with chronic pain requires a multifaceted approach. Mindfulness practices, cognitive-behavioural therapy (CBT), and medication management are effective strategies that can improve both cognitive and pain outcomes. Additionally, engaging in activities that stimulate brain function, like puzzles and social interactions, can provide cognitive benefits. By adopting a holistic plan that targets both pain and cognitive well-being, patients can achieve better overall health outcomes.
The Link Between Chronic Pain and Mood Disorders
Chronic pain and mood disorders, such as depression and anxiety, are often closely intertwined. Studies show that individuals with persistent pain are significantly more likely to experience mood disorders. This connection may be due to shared pathways in the brain that regulate both pain and emotions. The impact of ongoing discomfort on daily life can exacerbate feelings of sadness, worry, or hopelessness, highlighting the complex interplay between physical and emotional health.
How Chronic Pain Influences Mental Health
Experiencing chronic pain can take a heavy toll on one’s mental well-being. The constant battle with discomfort can lead to increased stress and emotional exhaustion, often worsening existing mood disorders. Furthermore, the limitations imposed by chronic pain, like reduced mobility and social isolation, can create a sense of helplessness and frustration. Understanding how pain influences mental health is crucial for developing effective treatment plans that address both physical and emotional symptoms.
Treating Both Pain and Mood Disorders for Better Outcomes
Treating chronic pain and associated mood disorders simultaneously can lead to improved health outcomes. Integrative approaches, such as combining pain management techniques with psychotherapy, have proven effective. Cognitive-behavioural therapy (CBT) can help patients manage the emotional impact of pain, while lifestyle changes, like regular exercise and mindfulness, can reduce stress and improve mood. By addressing both aspects together, patients can find greater relief and a better quality of life.
Understanding the Risk of Substance Abuse in Chronic Pain Sufferers
Chronic pain sufferers often face a heightened risk of substance abuse. The persistent discomfort may drive some to seek relief through pain medications, such as opioids, which can be highly addictive. Over time, the body builds a tolerance, leading individuals to consume higher doses and increasing the risk of dependency. This connection underscores the importance of careful monitoring and balanced pain management to minimise potential substance misuse.
Factors Contributing to Addiction Among Pain Patients
Several factors can make chronic pain patients vulnerable to substance abuse. Emotional distress, limited treatment options, and the stigmatisation of chronic pain conditions can lead individuals to self-medicate. Moreover, underlying psychological conditions, such as anxiety or depression, can exacerbate the desire to rely on drugs for relief. Recognising these contributing factors is key to developing comprehensive prevention and treatment strategies that address the root causes of addiction.
Effective Prevention Strategies to Mitigate Risk
Preventing substance abuse among chronic pain sufferers requires a holistic approach. Physicians can implement strategies like prescribing non-opioid pain management therapies and closely monitoring medication use. Multidisciplinary approaches, including physical therapy, cognitive-behavioral therapy, and mindfulness techniques, can also reduce reliance on medications. Education and support groups further empower patients to explore safer, more sustainable pain management methods, lowering the risk of substance misuse.
Cognitive-Behavioural Therapy (CBT) for Chronic Pain Management
Cognitive-Behavioural Therapy (CBT) is one of the most effective psychological therapies for managing chronic pain. This approach helps patients reframe negative thought patterns that can worsen the perception of pain. By teaching coping mechanisms and relaxation techniques, CBT empowers individuals to regain control over their pain experiences. Studies have shown that patients undergoing CBT report significant reductions in pain intensity and improved emotional well-being, making it a cornerstone of non-pharmacological pain treatment.
Mindfulness and Meditation for Pain Relief
Mindfulness and meditation have become popular strategies for reducing chronic pain symptoms. These therapies emphasize staying present and accepting pain without judgment, which can decrease emotional distress and improve overall quality of life. Techniques like guided meditation and mindful breathing help calm the nervous system and lower stress levels, which often amplify pain sensations. Integrating mindfulness practices into daily routines can provide lasting benefits and is a highly recommended complementary therapy for pain relief.
Acceptance and Commitment Therapy (ACT) for Pain Coping
Acceptance and Commitment Therapy (ACT) is another psychological approach that has proven effective for chronic pain patients. Unlike traditional pain management methods that focus on eliminating pain, ACT encourages patients to accept pain as a part of life while committing to meaningful activities. This therapy emphasises the importance of psychological flexibility, helping individuals find purpose despite their discomfort. By fostering a healthier relationship with pain, ACT can improve both mental and physical health outcomes.
Understanding the Grief and Loss Associated with Chronic Pain
Living with chronic pain often triggers feelings of grief and loss, as individuals mourn the life they once had before pain became a constant companion. The inability to engage in previously enjoyed activities or fulfill daily responsibilities can lead to a profound sense of loss. This grieving process can be similar to mourning a loved one, encompassing stages of denial, anger, and sadness. Recognising these emotions as a normal response to chronic pain is the first step toward healing.
Why Chronic Pain Can Deepen Emotional Distress
The emotional impact of chronic pain extends beyond physical discomfort, often leading to depression and anxiety. The realisation that pain may persist indefinitely can amplify feelings of hopelessness, and the societal misunderstanding of invisible illnesses may further isolate sufferers. This emotional distress compounds over time, making it critical for individuals to address their grief and seek support. Acknowledging the emotional toll of pain helps create space for coping mechanisms and a path forward.
Effective Coping Strategies to Manage Grief and Loss
Managing grief and loss due to chronic pain requires a holistic approach that addresses both emotional and physical aspects. Techniques like journaling, counseling, and joining support groups can provide a sense of community and emotional relief. Engaging in gentle exercise, practicing mindfulness, and setting realistic goals can also help restore a sense of purpose and agency. By embracing these strategies, chronic pain sufferers can navigate their grief and foster a renewed sense of well-being.
How Chronic Pain and Personality Disorders Are Linked
Chronic pain and personality disorders are interconnected in complex ways, with research indicating that one can exacerbate the other. Personality disorders, such as borderline or avoidant personality disorder, can influence how individuals perceive and cope with pain. People with certain personality traits, like high neuroticism or emotional instability, may experience pain more intensely or struggle with effective pain management. This bidirectional relationship underscores the need to approach pain treatment holistically, considering psychological factors.
The Psychological Impact of Chronic Pain on Personality
Living with persistent pain can have profound psychological effects, sometimes exacerbating underlying personality disorders. Chronic pain often increases emotional distress, leading to heightened symptoms of personality disorders, such as impulsivity or social withdrawal. Additionally, the frustration and limitations imposed by pain can strain relationships and worsen self-esteem issues, especially in those predisposed to personality challenges. Understanding these effects helps clinicians develop more personalised and effective treatment strategies.
Treatment Approaches Addressing Both Pain and Personality Disorders
Treating chronic pain in patients with personality disorders requires an integrated approach. Psychological therapies, like Dialectical Behaviour Therapy (DBT), are particularly beneficial for individuals with emotional regulation difficulties. Pain management techniques, combined with counseling to address underlying personality traits, can improve overall quality of life. Effective communication between healthcare providers, including pain specialists and mental health professionals, is essential to ensure comprehensive and coordinated care for these complex cases.
Mental Health Counseling and Support Groups
One of the most valuable resources for chronic pain sufferers is access to mental health counseling. Therapists specialising in chronic pain management can help patients develop coping strategies, address feelings of depression or anxiety, and improve overall emotional well-being. Support groups, both in-person and online, also offer a sense of community and understanding. Connecting with others who share similar experiences can reduce feelings of isolation and provide practical tips for managing the emotional impact of chronic pain.
Mindfulness and Relaxation Programs
Mindfulness-based stress reduction (MBSR) programs have become increasingly popular among chronic pain sufferers. These programs teach techniques like meditation, deep breathing, and gentle yoga to reduce stress and enhance mental clarity. Many hospitals and wellness centers offer structured mindfulness courses specifically designed for individuals dealing with chronic pain. Mobile apps and online platforms also provide guided relaxation exercises, making these resources easily accessible to those seeking relief and mental health support.
Educational Resources and Self-Help Books
Educational resources play a critical role in empowering chronic pain patients to take charge of their mental health. Websites like the American Chronic Pain Association and National Pain Report offer articles, research updates, and practical advice on living with chronic pain. Self-help books focusing on cognitive-behavioral techniques, such as “The Pain Management Workbook,” can guide readers through actionable steps for improving mental well-being. These resources equip sufferers with knowledge and skills to better manage both their physical and emotional challenges.
Harnessing Neuroplasticity to Improve Mental Health and Reduce Chronic Pain
Neuroplasticity, the brain’s ability to reorganise and form new neural connections, plays a crucial role in managing chronic pain and improving mental health. Through targeted interventions, the brain can “rewire” itself to reduce the intensity of pain signals and strengthen positive mental patterns. Here are some ways to harness neuroplasticity for these benefits:
Mindfulness and Meditation: Practices like mindfulness meditation have been shown to promote neuroplasticity. Regular mindfulness training can decrease the brain’s sensitivity to pain and foster emotional regulation. This process enhances gray matter density in regions associated with self-control and reduces activity in areas responsible for pain perception. As a result, individuals experience less pain and improved mental clarity.
Cognitive-Behavioural Therapy (CBT): CBT utilizes the concept of neuroplasticity to reshape negative thought patterns. By repeatedly practicing healthier thinking and behavior, the brain forms new pathways that reduce emotional distress and pain perception. This therapy helps break the cycle of chronic pain and mental health issues by reinforcing neural circuits that promote resilience and optimism.
Physical and Mental Exercise: Engaging in physical activities like yoga and aerobic exercise stimulates neurogenesis (the creation of new neurons) and strengthens neural connections. Mental exercises, such as learning new skills or solving puzzles, can also boost cognitive flexibility and improve brain function. Combining physical and mental activities helps reduce chronic pain by shifting focus away from pain and enhancing overall well-being.
By understanding and utilising neuroplasticity, individuals can take proactive steps to manage chronic pain and elevate their mental health, leading to a higher quality of life.
The Strain of Chronic Pain on Family Relationships
Chronic pain doesn’t just affect the individual experiencing it; it can significantly impact family dynamics. The emotional and physical toll of persistent pain may cause mood swings, irritability, and reduced participation in family activities. This strain can lead to misunderstandings, frustration, and even resentment among family members. Spouses or children may take on additional responsibilities, which can create feelings of imbalance and exhaustion within the household, making it crucial to address these changes head-on.
Communication Is Key to Reducing Tension
Open and honest communication is essential for maintaining healthy family relationships when dealing with chronic pain. Sharing feelings, concerns, and limitations helps family members understand each other’s experiences and fosters empathy. Regular family meetings or check-ins can provide a safe space to discuss adjustments and express appreciation for one another’s support. Active listening and validation of emotions can go a long way in reducing tension and strengthening bonds, even in challenging circumstances.
Strategies to Maintain a Balanced and Supportive Family Environment
To keep family relationships strong, it’s important to adopt strategies that promote balance and support. Establishing clear boundaries and distributing household responsibilities fairly can prevent caregiver burnout. Engaging in enjoyable activities that accommodate the individual’s pain levels, such as movie nights or gentle walks, can help maintain a sense of connection. Additionally, family therapy or support groups can provide valuable resources and coping mechanisms, ensuring that everyone in the household feels seen and heard.
The Importance of Resilience in Managing Chronic Pain
Building resilience is crucial for those dealing with chronic pain, as it equips individuals with the mental strength needed to navigate ongoing challenges. Resilience doesn’t eliminate pain, but it helps lessen the emotional impact, making it easier to cope with day-to-day difficulties. Research has shown that people with higher resilience levels are better at managing stress and maintaining a positive outlook, even when facing persistent discomfort. This strength creates a solid foundation for better overall well-being.
Developing a Growth Mindset to Strengthen Mental Health
A growth mindset, or the belief that one can adapt and improve over time, is a key aspect of building resilience. Chronic pain sufferers who focus on what they can control, like learning new coping strategies, often experience improved mental health. Techniques such as positive self-talk, goal setting, and celebrating small victories can shift focus from limitations to possibilities. Adopting this mindset encourages perseverance and self-compassion, both essential for long-term emotional and physical wellness.
Practical Strategies to Foster Resilience and Reduce Pain’s Impact
There are several effective ways to build resilience and reduce the impact of chronic pain on mental health. Engaging in regular physical activity, such as gentle yoga or swimming, can boost endorphin levels and improve mood. Practicing mindfulness meditation helps manage pain by calming the mind and reducing anxiety. Additionally, surrounding oneself with a supportive community, whether through friends, family, or support groups, provides emotional stability and motivation to keep moving forward. These strategies together create a strong defense against the challenges of chronic pain.